40 year old male with cough associated with sputum and dyspnea.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welc
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Icu bed 2
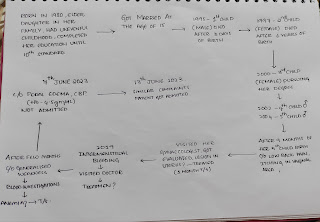
40 year old male resident of guntepalli came to OPD
Chief complaints:
Cough associated with blood since 10 days
Breathlessness since 10 days.
History of presenting Illness:
Patient was apparently asymptomatic 10 days ago.Then he developed cough which is associated with blood ,non foul smelling, approximately 10 times a day(approximately 5-10 ml in a day)not associated with clots.
H/o breathlessness since 10 days ( grade 4 acc to NYHA Classification .
H/o swelling in the limbs and face since 1 month .
H/o palpitations .
No H/o chest pain ,Chest tightness.
Daily routine:
Patient wakes up around 6-7 am ,does his daily activities.He will drink tea ,have breakfast by 8 am.Then he leaves for his work which is to collect old metal things and seggregate the scrap .He will return to home by 1 pm. Hw will have lunch then separate the scrap he collected in the morning.later in the evening he takes rest.He will have dinner by 9 pm and sleep by 10 pm.
Past History:
4 year ago (2018)
He noticed a swelling in the neck region which is of lemon size, not associated with pain went to near by hospitals but not relieved.So ,he was referred to a higher centre,where he was diagnosed with papillary carcinoma of thyroid after undergoing certain investigations, he had total thyroidectomy.
On Thyronorm 100 micrograms since 4 years.
Not a k/c/o Diabetes Mellitus, Hypertension,Asthma, Epilepsy, Tuberculosis.
No H/o similar complaints in the past.
Personal History:
Normal appetite
Mixed Diet
Regular Bowel and bladder movements
Adequate sleep
He is a teetotaler quit smoking and drinking alcohol 10 years ago .
No allergies.
Family history:
No significant family history.
Treatment history:
Thyroxine 100 mcg
On presentation his vitals :
Temperature:97.8°F
Pulse rate : 98 bpm
Respiration: 20cpm
BP : 110/70 mm Hg .
General Examination:
Patient was conscious, coherent and cooperative.He was well oriented to time place and person.
Pallor present
No signs of icterus,cyanosis, clubbing, lymphadenopathy.
Generalised edema present at the time of presentation.
Respiratory system:
Inspection :
Shape of chest - elliptical
B/L symmetrical chest
Trachea central
Symmetrical expansion of chest
No drooping of shoulder
No crowding of ribs
Palpation:
No local rise of temperature
No tenderness
All inspectory findings are normal
Traches central
Chest movements equal on both sides
Apex beat - 5th inter costal space medial to mid clavicular line
Percussion :
Resonant
Auscultation :
Bilateral airway clear
Vesicular breath sounds heard
Cardio vascular examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs
CNS examination: No neurological deficit found.
Gait: normal.
Normal speech.
Per Abdomen :
Per abdomen:
Shape of abdomen: scaphoid
No tenderness
No organomegaly.
Bowel sounds not heard .
Investigations
On 19/12/22
Color Doppler
On 20 /12/22
HRCT
On 21/12/22
Provisional Diagnosis :
Heart failure due to reduced ejection fraction 2° to pneumonia or pulmonary edema .
Hemoptysis under evaluation
Total thyroidectomy for papillary carcinoma of thyroid.
Prerenal AKI with cardiogenic shock


























Comments
Post a Comment