34 year old male with pleural effusion.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 34 year old male works in a vegetable market (lifts heavyweight bags) resident of moosapet(Hyderabad) father of 1 daughter and 1 son came to OPD with chief complaints of
Breathlessness since 2 months
Burning sensation in abdomen since 1 month .
History of presenting illness:
Patient was apparently asymptomatic 2 months ago .Then he developed high grade fever which was insidious in onset , gradually progressive in nature associated with chills and rigors .It aggravated on performing daily chores and relieved on taking medication.
Fever is associated with severe body pains .
H/o cough Since 2 months which was insidious in onset non productive ,non blood stained,non foul smelling.no aggravating and relieving factors.
Breathlessness (SOB) started 2 months ago which was insidious in onset , relieved on sitting down position . Grade 2 acc to MMRC .
H/o burning sensation in the abdomen since 1 month which was insidious in onset , gradually progressive in nature , aggravated on intake of alcohol and spicy food , relieved on medication.It is recurrent in nature .
H/o 1 episode of vomiting which was non bilious,no projectile, contains food contents, relieved on medication.
H/o 1 episode of blood in stools .
H/o painful defecation.
No h/o orthopnea, paroxysmal nocturnal dyspnea.
No h/o chest tightness,chest pain, palpitations.
No h/o weight loss, sweating.
Daily routine.
Before onset of fever:
He used to wake up early in the morning.He drinks tea and get ready to leave for his work by 5 am to vegetable market.He will work(lifts bags) until 1pm in the market and returns home to have lunch.After having lunch,he will sleep until evening.He stays at home in the evening time and plays with his kids .Later during dinner he will have 1 cup of rice and curry and goes to sleep.
After onset of fever:
He started having fever and severe body pains which didn't let him to do his work .So he stopped going to work and stayed at home since 2 months
Past history:
Not a k/c/o Hypertension,Diabetes mellitus,Thyroid disorders, Asthma, Tuberculosis, Epilepsy,Coronary artery disease.
Personal History:
Mixed diet
Reduced appetite (since 2 months)
Adequate sleep
Regular bladder movements
Bowel movements irregular (constipation since 5 months)
Addiction:
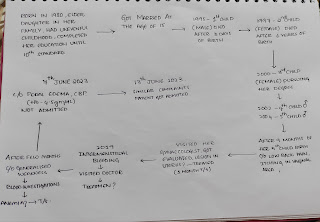
Alcohol intake since 2006 (90ml per day) due to peer pressure ,but chronic alcoholic since 2018 (increased 4 fold) when his wife left home for delivery.
Tobacco consumption since 2008(1 or 2 per day) but increased smoking since 2018 ( 20 cigarettes per day)
Family history:
No significant family history.
General examination:
Patient was coherent , conscious, cooperative.
He is well built and well nourished.
No signs of pallor,icterus,cyanosis, clubbing,lymphadenopathy,edema.
Vitals
Temperature:afebrile
Blood pressure:120/80 mm Hg
Respiratory rate :16cpm
Pulse rate:75bpm
Systemic examination:
Inspection:
No structural abnormalities in nose, no obstruction in nasal airway .
Oral cavity - no crooked teeth
Pigmented patches present on tongue .
No ulcers in mouth.
Trachea appears to be central.
Bilateral symmetrical.Elliptical in shape.
Symmetrical expansion on both sides.
No scars ,sinuses,engorged veins.
Palpation:
No local rise of temperature
No tenderness.
Trachea is central.
Anterioposterior diameter - 19 cm .
Transverse diameter -28 cm .
Apex beat present in medical to mid clavicular line in 5th intercostal space.
Chest expansion equal on both sides.
Tactile vocal fremitus present on both sides.
Percussion.
Auscultation:
Per abdomen examination:
On inspection
Shape of abdomen : flat
Umbilicus : inverted
Movements of abdomen wall with respiration
No visible peristalsis, pulsations, sinuses, engorged veins, hernial sites
On palpation
No local rise of temperature
Inspectors findings are confirmed
Soft and non tender
No palpable mass
Liver and spleen not palpable
On percussion
Resonance note heard
On auscultation
Bowel sounds heard
CVS examination:
S1 S2 heard
No murmurs heard
CNS examination :
No focal neurological deficits found.
Investigations:
Complete Blood picture
Hemoglobin -16.7mg/dl
Total count - 3300 cells/cumm
Neutrophils - 65%
Lymphocytes - 19%
Eosinophils -1%
Monocytes - 15 %
Basophils -0%
Platelet count -1.24 lakh
SMEAR - normocytic normochromic blood picture
Liver function tests
Total bilirubin -1.37 mg/dl
Direct bilirubin -0.23 mg/dl
AST -64 IU/L
ALT -32 IU/L
Alkaline phosphate - 310 IU/L
Total proteins: 7 mg/dl
Albumin - 3.43 mg/dl
A/G ratio -0.96
Chest USG :
Findings
Free fluid noted in left pleural space with underlying lung collapse
Right pleural space normal
No consolidation seen in both lungs
No collapse seen in right lung
Diagnosis :
Minimal pleural effusion on left side.











Comments
Post a Comment