MY EXPERIENCES WITH GENERAL CELLULAR AND NEURAL CELLULAR PATHOLOGY IN A CASE BASED BLENDED LEARNING ECOSYSTEM'S CBBLE
Hello ,I am Chittireddy Asritha , final year medicine student from India. I am here to share my journey in the department of medicine . When I started attending clinical postings regularly I came to know that there are lot of things that are seen , felt or understood only after interacting with patients . With the help of my seniors , residents and professors I learnt how to take a detailed history, examine patients and diagnose a patient. I am committed and dedicated to continuous learning , and effective communication with my patients , colleagues, seniors, professors to provide the best health care to my future patients .
One thing that I learnt in my journey is to take the detailed history of a patient which will almost lead us to the system with abnormal pathology. It is also mentioned by our professors in clinical rounds that constant interaction with the patient will let us understand the condition of the patient in a better way to diagnose and treat the condition.
"JUST LISTEN TO THE PATIENT, HE IS TELLING YOU DIAGNOSIS " - Sir William Osler .
UNDERSTANDING >>>>>>>>> MEMORISE
NOTE: THIS IS AN ONLINE E LOGBOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS/HER GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS INTENDING TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
FIRST CASE : 55 year old female with abnormal glucose levels.
Patient Complaints:- Patient was apparently asymptomatic 2 years ago. On one fine day while she was doing her household work she had giddiness which lasted for a while and has been taken to a nearby hospital .She gave a history of increased frequency of urine since 1monthH/o generalised weakness since 15 days .H/o increased thirst (polydipsia) since 1 week .H/o vomitings 4 days ago (3 times/ day ) food as content,non projectile in nature,non blood stained . After routine blood and urine investigation she was diagnosed with diabetes mellitus and was on medication since then.(Tab .Metformin 500 mg )
On the date of admission,
Diminishing of vision since 6 months in the left eye and was posted for surgery ,but her glucose levels were abnormal so referred for control of glucose levels to bring down to normal levels .No H/o loss of sensation in limbs.(upper and lower)No H/o tingling sensation in limbs.No H/o swelling in ankles ,feet, hands and legs.
Since she was referred for control of blood glucose levels she was monitored before and after intake of food for glucose levels. Then we found out that there was peculiar pattern of rose and fall of blood glucose levels i.e., there is low blood sugar levels during nights and high rise in blood sugar levels in the morning .
Then , i approached my senior " sir, what could be the reason behind this rise and fall of levels!?" Then he replied " Have u heard of somogyi effect?" . My answer was "No " . Then he explained me that this effect happens when a high blood glucose in the morning is lead by the low blood glucose in the night due to Hormones.It happens after insulin intake.So this pattern in this patient could be probably because of somogyi effect where she suddenly becomes hypoglycemic and feels dizziness. Later he also gave a brief description of Dawn phenomenon.
Later she was kept on insulin with adjusted timings and doses and blood glucose levels were controlled and posted for eye surgery for her diminished vision.
55-year-old-female-with-uncontrolled.html?m=1
In this case something what fascinated me was that I never heard about somogyi effect and dawn phenomenon while I was learning about diabetes mellitus in my previous years.
Dawn phenomenon happens when hormones your body naturally makes in the early morning (including cortisol and growth hormone) increase your blood sugar.
The Somogyi effect also involves a surge of hormones, but it's due to a low blood sugar episode overnight that leads to high blood sugar levels in the morning.
https://www.ncbi.nlm.nih.gov/books/NBK551525/
Second Case :
During my clinical postings in my final year , i came across this 23 year old lady in the medical ward . I approached her and introduced myself and requested her if she could share about the reason for her admission in the hospital.Patient replied " I am 23 years old , After I woke up in the morning my face becomes puffy and there is also swelling in my both limbs " .
Qsn: How long has it been you have noticed this symptoms?
Patient: It's been 5 months on and off . I have been on medication but it is recurrent.
Then i further asked her about the detailed history -
On further examination of patient there was pitting type of edema , periorbital edema . No other positive findings on Systemic Examination.When we further investigated the patient her complete Blood picture was normal,Serum creatinine was normal ,no positive findings in urine analysis.
So 24 hr urine protein , creatinine were monitored and the results were as follows which were quite higher than the normal levels
24 hr urine protein - 5,233 mg/ day
24 hr urine creatinine - 5.5 gm / day
As we know that elevated urine protein levels are indicating that there is decreased protein levels in the blood due to dysfunction of glomeruli (glomerular injury ) which lead to decreased colloidal osmotic pressure that leads to increased aldosterone secretion , inturn leads to sodium and water retention that leads to edema
After,further investigations she was diagnosed with Nephrotic syndrome.She was on following medication and monitored for fluid and salt restriction.
Tab.Lasix 20 mg PO BD
Tab .Ramipril 2.5 mg PO/OD
https://chittireddyasritha32.blogspot.com/2022/11/23-year-old-female-with-facial.html?m=1
Learning points:
Difference between Nephrotic and Nephritic syndrome
Etiology and pathophysiology of Nephrotic syndrome
Pathophysiology of edema in Nephrotic syndrome : I got to know that there are two hypothesis ( under fill and over fill)after going through following article.
Approach towards a case of Nephrotic syndrome.
https://www.niddk.nih.gov/health-information/kidney-disease/nephrotic-syndrome-adults
Third case -
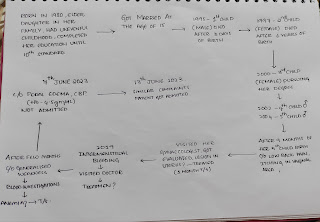
This is another case that I came across in my final year ,32 year old male who was on bed suffering with high fever associated with chills and rigors.Then , i approached patient but he was feeling weak and unable to explain about himself. So, I asked his wife then she started explaining how and when his illness started as follows :
Patien was suffering from fever ,cough ,abdominal pain (RUQ) since 1 week . I took detailed history and further proceeded with examination based on the history provided.So, I explained about how examiner is done and took consent from the patient. Upon examination reduced vocal fremitus on rt side in Mammary,Inframammary,Suprascapular regions.On percussion,dullness is noted on rt side .On auscultation breath sounds are not heard in Mammary, Inframammary, Axillary and Infra Axillary Regions. In X-ray there was clear obliteration of costophrenic angle .Pleural tap was done for two times. So the patient was being treated for mild pleural effusion and confirmatory tests were ordered.Since his fever was persistent for 4 days, then we suspected could there be an infection?When pleural tap was sent for CBNAAT ,it turned out to be positive . So the patient was put on Anti tubercular Drug regimen and was advised for follow up. The blog can be found below:
https://chittireddyasritha32.blogspot.com/2023/04/32-year-old-male-with-pleural-effusion.html?m=1
While doing rounds during clinical postings,i learnt how our residents tried to explain and pacify the family of a TB positive patient , how to take care of him and measures to be followed ( ex:- using mask) . Patient was also explained about the side-effects of the drugs in the regimen and was advised to immediately come to op if any of them were severe( ex - Rifampicin - orange colour fluids ; Ethambutol- regular ophthalmology check-up; ) .
Learning points :
✓ causes of pleural effusion
✓ How do we differentiate Transudative and Exudative pleural effusion
✓ Lights criteria in pleural effusion
✓ Relation between TB and pleural effusion.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4958858/
TPE predominates in men, with an overall male-to-female ratio of 2:1 In an epidemiological analysis from the United States, TPE occurs significantly more often than pulmonary tuberculosis among persons >65 years old, and the mean age of patients with TPE is 49 years: about 50% were younger than 45 years and 30% were over 65 years of age . In contrast, TPE affects mainly younger individuals (mean age =34 years) in higher tuberculosis burden areas, where primary infection accounts for a large percentage of patients with TPE
TPE usually manifests as an acute illness, especially in younger patients who are more immunocompetent. Upon presentation symptoms in one series had been present for less than a month 50/71 patients (71%) and had been present for less than 1 week in 25/71 patients (35%) . The most frequent symptoms of TPE are nonproductive cough and pleuritic chest pain; if both cough and chest pain are present, the pain usually precedes the cough . Most patients are febrile but approximately 15% will be afebrile. Dyspnea can be present in some TPE patients if the effusion is large. Other symptoms include night sweats, weight loss, malaise .
TPE is usually unilateral and can be of any size. In our series of 333 patients, pleural fluid occurred only on the left side in 127 (38.1%), only on the right in 161 (48.4%), and both sides were affected in 45 (13.5%) . In either unilateral or bilateral effusion, the percentages of small, moderate, and large size of pleural effusions were 20.4%, 19.2%, and 60.4%, respectively . Approximately 20% of patients with TPE have coexisting parenchymal disease on chest radiograph . However, computed tomography scanning offers a more sensitive method and can demonstrate parenchymal disease in 40–85% of cases.
I would like to express my vote of thanks to my esteemed Professors, Residents and my colleagues in the Department of Medicine for their effortless teaching , mentoring and guiding us to improve our understanding the concept and learning skills which is leading us to become compassionate and skilled physicians.


Comments
Post a Comment