32 Year old male with C/O aphasia and generalised weakness
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
32 year old male resident of chityala came to casualty with c/o
generalised weakness since 2 days
difficulty in talking since 2 hrs
ECG on 18/1/2024
HOPI :
Patient was apparently asymptomatic 2 hours ago . He started to have difficulty in talking since 2 hours (Acc to pt he started having it after having soft drink ) .
No h/o deviation / angulation of mouth
No h/o deviation of tongue
No h/o nausea, vomiting and head ache
No h/o tingling sensation in limbs
No h/o perioral numbness
No h/o slurring of speech .
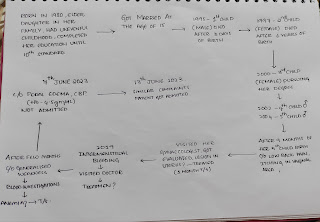
Past history :
Patient had two episodes of seizures in past
1) When patient was in seventh standard he got an electric shock and was immediately taken to hospital for treatment and recovered.Later after 3-4 days after this incident patient had an episode of seizures , associated with weakness of limbs and foam from mouth + .No h/o tongue bite , deviation of tongue , angulation of mouth ,perioral numbness at night when he was asleep and was taken to hospital, treated accordingly and used medication for 3 months .
2) 2 nd episode of seizures was seen around 1 month ago around 10 pm at night ( he was in an yoga ashram near srisailam ) which was observed by people around him and immediately they kept keys in his hands and it resolved after half an hour. He was told that he didn't need to go to hospital by those elders in ashram as he was doing yoga and doing meditation regularly.
At the time of episode - H/o tongue bite present on the left side , weakness in both limbs present .
No h/o angulation of mouth
No h/o tingling sensation in limbs
No h/o perioral numbness
No h/o slurring of speech .
No h/o fever , sweating
No h/o nausea , vomiting
No h/o headache
After he came from aashram he went to near by hospital in nalgonda and they advised to get an MRI and gave medication . He neglected it at that time . But since he started having weakness in both upper and lower limbs since 2 days and slurring of speech since 2 hrs he decided to come and get an MRI done at our hospital.
Patient got COVID 2 times in 2020 and 2021 respectively .
1 ) In 2020 he firstly had loss of taste , got tested turned to be positive and took medication ( Azithromycin, Vitamin C , Hydroxychloroquine ) from government for 15 days ( quarantine) he recovered well.
2) In 2021 he again got COVID had similar symptoms like the previous one and took medication provided by government and recovered.
Later he got 2 doses of COVID vaccine .
H/o bilateral hip pain , neck pain (on and off ) since 2 years and visited hospital 2 weeks they have advised him to get an x ray and reported it as ? loss of lumbar lordosis and advised medications for the same .
He had diminished of vision in both eyes since 1 year , got a check up from an ophthalmologist and they diagnosed it as a cataract and advised him to get his surgery done. Six months ago he underwent cataract surgery for his left eye.
N/k/c/o DM, HTN , Asthma , TB, Thyroid disorders
Personal History :
Appetite - normal
Diet - Mixed diet
Bowel and bladder - regular
Sleep - Adequate
Alcohol ( beer ) consumed occasionally (2 bottles ) but at the age of 15 years and stopped at 28 years of age
He simultaneously started smoking ( 1/2 per day ) while taking alcohol along with friends but stopped at the age of 20 .
No significant family history.
General Examination:
Patient is conscious, coherent, co-operative
Well nourished,well built .
No signs of pallor , icterus, cyanosis, clubbing, lymphadenopathy.
Hyperpigmented lesions present over trunk and both limbs
Vitals :
Blood pressure 120/80 mm hg
Pulse rate - 108 bpm
Respiratory Rate - 18cpm
Temperature - 98.6 °F
Grbs : 128 mg / dl
Trousseau's sign. -positive
Chvostek sign - postive
Systemic Examination :
CNS EXAMINATION:
Patient was unconscious at the time of presentation and aphasic
Cranial nerves examination - Intact
Motor system
Right. Left
Tone :
Upper limb Normal. Normal
Lower limb Normal. Normal
Power :
Upper Limb. 5/5. 5/5
Lower Limb. 5/5. 5/5
Reflexes: biceps. Mute. Mute
Triceps. Mute. Mute
Supinator. Mute. Mute
Knee. Mute. Mute
Ankle. Mute Mute
Plantar. Flexor. Flexor
Sensory Examination : No abnormalities detected
Meningeal signs - absent
Finger nose coordination - absent ( at the time of presentation)
Knee heel coordination - absent ( at the time of presentation
PER ABDOMEN EXAMINATION :
On inspection
Shape of abdomen : flat
Umbilicus : inverted
Movements of abdomen wall with respiration
No visible peristalsis, pulsations, sinuses, engorged veins, hernial sites
On palpation
No local rise of temperature
Inspectors findings are confirmed
Soft and non tender
No palpable mass
Liver and spleen not palpable
On percussion
Resonance note heard
On auscultation
Bowel sounds heard
RESPIRATORY SYSTEM
Inspection:
Trachea appears to be Central
shape of chest - elliptical
Movements of chest appear to be bilaterally equal
Keloid is present on chest in midline
No drooping of shoulder
No engorged veins , swellings seen
No hallowing seen
No crowding of ribs
Palpation:
All inspectory findings are confirmed
No rise of temperature
No tenderness
Trachea is central.
B/L chest movements are equal
No swelling and palpable masses are felt
vocal fremitus are normal
Apex beat is felt at 5th ICS 1cm medial to mid clavicular line.
Percussion:
Resonant note heard in all regions.
Auscultation :
Normal vesicular breath sounds heard.
CVS EXAMINATION
Inspection-
No raised JVP
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse at 5th intercostal space
Palpation-
Apex beat is felt in the fifth intercostal space, 1 cm medial to the midclavicular line
Percussion -
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
Provisional Diagnosis:
Generalised Tonic clinic seizures ? secondary to Hypocalcaemia
ECG on 16/1/2024











Comments
Post a Comment